Complaint
The complaint consists of pain in the Achilles tendon, usually about 2 to 6 cm above the heel bone. The pain usually develops gradually. Initially, the pain is felt only at the beginning and after the end of load, later also at rest. There is often swelling and morning stiffness. This injury mainly occurs in athletes of athletics, tennis, badminton and football, but also in people who have not played sports for a long time.
Condition
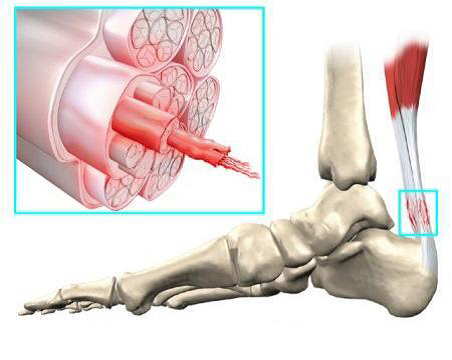
The Achilles tendon connects the calf muscles (m. gastrocnemius and m. soleus) to the heel. It is the thickest and strongest tendon in the human body. Previously, it was thought that Achilles tendon complaints were caused by an inflammatory process. It is now clear that this is not correct.
Examination of surgically removed tendon tissue revealed no inflammatory cells. However, the quality of the tendon tissue had decreased and the normal structure of the tendon had changed. This degenerative process leads to weakness of the Achilles tendon and is a response of the Achilles tendon to overuse or underuse.
Causes
A number of underlying factors can contribute to the development of Achilles tendon complaints. The complaints can be the result of properties related to the body (= intrinsic), but environmental factors (= extrinsic) can also play a role. Often, not one factor is responsible for the development of the complaints, but a combination of several

Intrinsic:
- Decreased blood flow to the tendon due to aging
- Decreased muscle strength, stability, and flexibility of the calf muscles
- Overweight
- Deviations in the shape of the foot, resulting in more walking on the inside of the foot and an asymmetrical
- load on the Achilles tendon.
Extrinsic:
- Changed exercise intensity
- Bad running technique
- Bad running shoes:
– Worn and therefore poor gait
– Shoes that do not suit the running style and foot shape
- Surface: a surface that is too hard or too soft (loose sand) or slippery can increase the load on the Achilles tendon.
Treatment
Correcting intrinsic and extrinsic factors is a first step. For example, measuring insoles, adjusting footwear, and the surface.
Exercise therapy:
- Eccentric exercise therapy: these are exercises in which the calf muscles are stretched while they are actively contracted under extension. Exercises should be performed once or twice a day for 12 weeks. Sometimes there is a short-term increase in pain at the beginning of the treatment, but this is not a reason to stop the exercises.
- Stretching exercises of the short and long calf muscles.
Medicines:
In the acute phase, anti-inflammatory drugs (diclofenac or ibuprofen) can reduce the symptoms. The aim is to relax the Achilles tendon in order to start exercise therapy. Good results have been reported with polidocanol injections and nitrate patches, but the scientific evidence of these forms of therapy is still very thin.
ACP (PRP) injections:
This is a promising technique in which blood is taken from the patient and then processed. The body’s own growth factors obtained in this way can be injected into the tendon where they can promote repair of the tendon.

Night spak of “Strassburg sock”:
Damaged tendon tissue is repaired during sleep. At night in bed, people usually lie with their toes pointing downwards. When one gets up in the morning, the newly healed tissue is broken again. This manifests itself as morning stiffness.
The night splint holds the ankle at a 90° angle and the Achilles tendon heals in the correct position. There are indications that a night splint can reduce pain and improve function. However, the treatment is quite burdensome and does not work for everyone.
Operation:
An operation can be considered if after 6 months of targeted treatment insufficient results have been achieved and there are many complaints and limitations. Two surgical techniques are described below:
- Percutaneous longitudinal tenotomy:
With the help of 2 to 3 small incisions, several cuts are made in the longitudinal direction of the tendon. - Open procedure:
Degenerative tissue is removed, after which tendon reconstruction takes place.
The success rates are between 75 and 80%. The recovery period is long (4-12 months).
Achilles tendinopathy and sport
It is advised to choose an alternative form of training (eg swimming, cycling or a strength program) to maintain fitness, strength and stability.
When morning stiffness and starting pain decrease and causal factors have been addressed, sports and training forms can be slowly built up again.
Preventing Achilles tendinopathy
The risk of an Achilles tendon injury can be reduced by paying attention to the following:
A good warm-up and cool-down of 10 to 15 minutes reduces the chance of an Achilles tendon injury. It is important to pay attention to the stretching exercises of the foot and calf muscles.
Especially at the beginning of the season, training too much, too often and too hard is a pitfall. A good training structure is important, whereby the scope of the training is first expanded (number of hours) and only then the intensity (intensive forms of exercise with a lot of running work).
Choose sports shoes that are suitable for the personal running style and foot shape. Very important is the stability around the ankle. Good advice from a specialist shop is very valuable here. The average life of a sports shoe is 500 to 750 kilometers. After this, it quickly loses its shock-absorbing effect.
Sometimes the body has certain shortcomings (think of foot shape defects). When these are recognized and corrected in time, unnecessary injuries can be prevented.
Wil je teruggebeld worden?
Door het invullen van het contactformulier ga je akkoord met onze privacy policy.
